When incarcerated people enter the healthcare system, the treatment they receive, or lack thereof, has consequences that extend beyond their cells and into the very question of who is seen as worthy of care. Interviews with a nursing manager who works at a well-known hospital and former California corrections inmate reveal a shared understanding: behind bars, access to healthcare is not just about medicine, but about the dignity of being seen as human in the first place. These two voices, from different sides of the system, illuminate a healthcare crisis where structural gaps and social biases reinforce each other, leaving incarcerated patients to navigate a system that was never built to truly care for them.
The nursing manager, Gayle, described how the system’s failures are built into every step of care. From the moment an incarcerated patient enters the hospital, there are barriers: missing medical records, incomplete histories, and lack of preventative care. “There is often a disconnect between what’s available in the facility and what they need when they come to us,” she explained. This isn’t just an administrative hiccup; it’s a symptom of a deeper neglect that leaves incarcerated people without continuity of care or a basic sense of safety. Gayle’s perspective reveals how these gaps create an environment where patients are treated as numbers, not people; an environment that fails to recognize the basic rights of patients who are still paying for past mistakes.
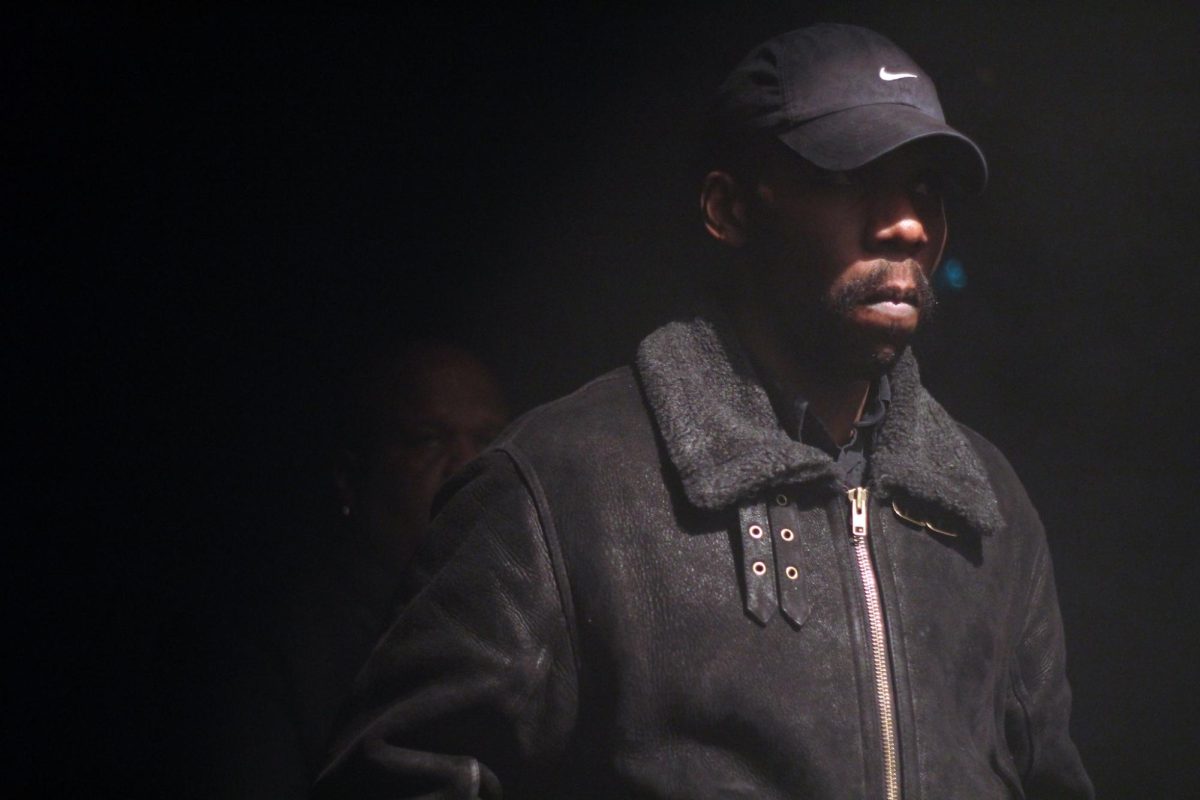
While the nurse sees the structural challenges from a professional distance, the former inmate knows them firsthand and front row. He described how even routine medical issues became a battle for attention and recognition. “It felt like we weren’t even human to them,” he told me bluntly in our interview. His stories of untreated infections and dismissed pain show how the system’s failures become personal wounds. But more than that, they reveal how the experience of incarceration strips away the expectation of dignity in healthcare. When the former inmate talked about the racial and class disparities he witnessed, it was clear these were not isolated failings; they were built into the system itself, creating a hierarchy of whose pain matters and whose doesn’t matter at all.
Even though both interviewees brought to light the systemic neglect, the inmate uncovers a more compounded mistreatment that is a reflection of the disservice of the many systems in our society: the healthcare system, the corrections system, the judicial system, and civil rights. “You don’t see the white inmates treated the same way…even the Asian inmates I feel had it a lil’ easier too,” he said. “It’s always Black and Brown guys being told to wait or just ignored and pushed over.” His account is backed by so many other public stories we have rubbed shoulders with over the years in movements like #BlackLivesMatter (BLM) that initiated in 2013 and is still ongoing; or the Black vs Blue (Black lives vs. law enforcement) rallies from 2020- 2023. The neglect and mortality for people of color, especially incarcerated, is much higher. Not just a mere issue of being under-resourced or low-funded as politicians portray, these issues are a repressed exposure of how racial bias intersects with corrections and healthcare, creating severely unequal outcomes.
The gap between these two perspectives, the professional and the personal, brings to apex a painful truth: what the nurse sees as gaps in records or policies, the former inmate experiences as a denial of humanity. Their voices echo on the same point: healthcare for incarcerated people is an afterthought, a checkbox, rather than a fundamental right. Even when care is technically provided, the quality and compassion of that care is shaped by a belief that these patients are somehow “less deserving.” This isn’t just a healthcare crisis…it’s a social one, with real consequences for public health and for how communities heal and rebuild after incarceration.
The nurse also revealed another hidden and detrimental aspect of caring for incarcerated patients: moral strain. “It’s hard,” she admitted. “You want to treat everyone with the same intent, but there’s pressure all around… security watching, assumptions being made about the inmate.” Her words reflect how there is without a doubt an internal conflict, one that many healthcare professionals face…. and that’s trying to uphold medical ethics in an environment shaped by criminal justice procedures and priorities. Situations like this can significantly distort how care is delivered, especially when the ones on board to impose these limitations are right in the room watching… like the hospital administrator or correctional officers micromanaging the care medical professionals give to inmates. Experiences like nurse Gayle’s shows that the true and necessary reform has to go beyond vocational training, but also a change in institutional practices that open the doors for implicit bias and selective assistance.
These interviews also highlight the way that public perception shapes policy and practice. The nurse spoke about how the stigma of incarceration can seep into healthcare itself, making it easier for policymakers to justify budget cuts or limited access. The former inmate’s stories show how that stigma becomes a daily reality. The fact that incarcerated people face worse outcomes for chronic illnesses, mental health issues, and even routine infections isn’t just a matter of bad luck; it’s a reflection of how our society decides whose lives are worth saving.
The consequences of this neglect doesn’t end when someone’s sentence does. As the former inmate explained, the untreated health issues he carried out of prison continue to shape his life today. The nurse sees this too: patients who were once incarcerated come back to the hospital with conditions that should have been treated. years ago. This revolving door between the corrections system and the healthcare system affects not only individuals but entire communities. It reinforces cycles of poverty and poor health, creating a public health crisis that spills over long after the bars have closed behind them.
As I listened to both interviewees, I began to understand that changes needed for situations as pernicious as the ones they have witnessed must start with policies and procedures being put in place, and then reinforced through practice. Nurses like Gayle have to do more than just “treat” inmates; in the background, they also have to advocate for more integrated communication between hospitals and correctional facilities. Her direct experience notes that communication and equality are not the only downfalls either, as the need for more experienced and trauma-informed staff also has its effects. The former inmate however, believes that the change starts with accountability: “There’s no one watching them. No one makes sure the care is real.. or enough. How do officers know what is enough…they didn’t go to school for medical stuff.” His words paint the larger picture of correctional healthcare: without oversight, reforms remain performative. Beyond accountability, the inmate also believes compliance is also a thing of the past. In his words, we need external review boards, we need consistent health audits, and we need legal protections for incarcerated patients. Simply put, we need a system designed to see that prisoners are patients too, not just medical inconveniences.
Beyond policy failures, stigmatic views also play a morbid role in the declination of healthcare quality behind bars. The former inmate said, “It’s like they decided who I was before I even opened my mouth. You’re not a patient…or even a person really. You are just another problem.” This treatment strips incarcerated people of any feeling of dignity or humanity, and can totally reshape their access to care. Even trained professionals, as corroborated by nurse Gayle, can fall into the trap of assuming less urgency or less empathy and thinking it’s justified due to the inmate’s status. Per Gayle, “There’s an unspoken tone…you know when a nurse or CNA has a mentality of ‘whatever, they’re just a prisoner anyways’.”
What happens inside correctional healthcare systems doesn’t stay confined to the prison walls. Many incarcerated individuals return to their communities with chronic conditions left untreated or worsened by neglect. As nurse Gayle states, “We see it on the outside when they come back through our ERs and Urgent Cares with preventable problems that I’m sure were ignored or downplayed inside wherever they were locked up.” This approach results in carceral neglect becoming a community burden, stretching public health resources, and reinforcing cycles of illness and instability. When a prison or jail health system fails, many people (not just the inmates) pay the price.
What these two voices reveal is that the healthcare in corrections isn’t just about medicine; it’s about the way we see and value people who are locked up. The nurse’s observations of bureaucratic gaps and the former inmate’s experiences of personal neglect both point to the same conclusion: without a fundamental shift in how we see incarcerated patients, these failures will continue. As the nurse said, “Everyone deserves healthcare,” but as the former inmate made clear, that ideal is far from reality. The question that remains is how we can change a system that treats incarcerated people’s lives as expendable, and what does it say about society if we don’t?”